Urinary incontinence—unintentional urine leakage—is a common and distressing complication faced by many men after prostate cancer treatments like prostatectomy (surgery), radiation therapy, or cryotherapy. While this side effect can affect your quality of life, the good news is that there are proactive steps you can take before and after treatment to improve bladder control and regain confidence.
At HFitness, we specialize in helping men recover and rebuild strength through targeted pelvic health programs. Here’s an introduction to urinary incontinence and prostate cancer treatment. This blog explains the causes of incontinence after prostate cancer, how common it is, and why pelvic floor therapy for men is an essential part of the solution.
Is Urinary Incontinence Common After Prostate Cancer Treatment?
Yes. Prostate cancer is one of the most frequently diagnosed cancers in men worldwide, and many undergo curative treatments like prostatectomy or radiation therapy. Both treatments can unfortunately impact the muscles and nerves involved in urinary control.
Studies estimate incontinence rates range from 5% to 30% after prostate surgery. The variation stems largely from how “incontinence” is defined. For instance:
-
Some studies define “continence” as using 0–1 pad per day.
-
Others only consider men continent if they have zero leakage and use no pads at all.
These differences in definitions explain why reported rates vary widely.
Why Does Incontinence Happen After Prostate Surgery?
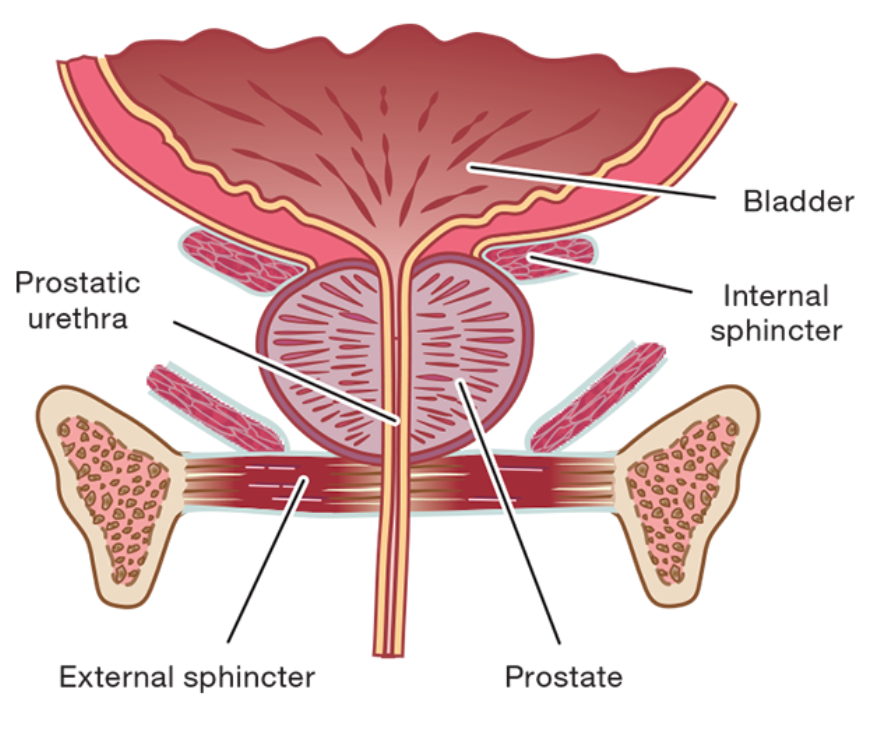
The prostate gland is situated near the urinary sphincter, which is a key muscle responsible for bladder control. During surgery or radiation, it’s often challenging to treat the prostate without weakening the sphincter muscle or affecting the surrounding nerves.
Even with precise surgical techniques, some degree of trauma to these muscles is common—leading to stress incontinence, the most frequent type of leakage experienced after treatment.
Why Do Incontinence Rates Vary So Much?
Definitions matter. Some doctors define incontinence as needing more than one pad per day, while others define continence as no leakage, ever. This inconsistency skews how “success” is measured after treatment.
Types of Incontinence: Not All Are the Same
Not quite. Incontinence can be:
-
Mild (occasional leakage)
-
Moderate (regular leakage with physical activity)
-
Severe (constant leakage or urgency)
The most common type after prostate treatment is stress incontinence, caused by weakness in the urinary sphincter — the muscle responsible for keeping urine in.
1. Stress Urinary Incontinence
This occurs when physical activity—like coughing, sneezing, lifting, or exercising—puts pressure on the bladder and leads to leakage. It is typically the result of sphincter weakness and is the most common form of incontinence after prostate surgery.
👉 Struggling with this type? Start recovery with our evidence-based
Prostatectomy Rehabilitation Program, designed specifically for men healing from surgery.
2. Urge Urinary Incontinence
This form is characterized by a sudden, intense need to urinate followed by involuntary leakage—often before reaching the bathroom. It may also involve symptoms like urinary frequency and nighttime urination.
👉 Get tailored support with our
Overactive Bladder and Urge Incontinence Program for Men to manage urgency and regain control.
What About Radiation or Cryotherapy?
While most men associate incontinence with prostate surgery, other treatments like radiation and cryotherapy can also lead to leakage. Radiation may irritate the bladder lining and weaken surrounding tissues over time, contributing to both stress and urge incontinence.
That’s why it’s important to have a long-term pelvic floor strategy, regardless of the treatment type.
Explore our full Men’s Pelvic Health Program Catalog to find the right solution for your situation.
Why Is Stress Incontinence So Common After Prostate Surgery?
Because the prostate gland sits next to the urinary sphincter, removing or treating it with radiation often affects this delicate area. Even highly skilled surgeons must balance removing cancerous tissue while preserving sphincter function.
What Is Stress Incontinence?
Stress urinary incontinence is leakage that occurs when pressure is placed on the bladder — like during coughing, sneezing, lifting, or exercising. It’s directly linked to weakened pelvic floor muscles or sphincter damage. This type of incontinence is especially common in men post-prostatectomy and is one of the most frustrating symptoms to manage.
Another type is urge incontinence, which involves a sudden, intense urge to urinate — often too fast to reach a bathroom. While urge incontinence is less common post-prostate treatment, some men may experience both types.
Can You Prepare Before Prostate Treatment?
Absolutely. Bladder health before treatment is key to post-treatment outcomes.
Start by asking your doctor:
-
What are the incontinence rates for your procedure?
-
What support is provided for recovery?
Then, begin pelvic floor strengthening exercises before surgery. By learning how to properly engage the right muscles, you’ll speed up recovery and improve your chances of maintaining bladder control.
👉 Explore Pelvic Floor Therapy for Men at HFitness
Our program is designed to help men prepare before treatment and recover afterward, using proven techniques that strengthen the pelvic floor and reduce leakage.
Final Thoughts: You’re Not Alone—And You Can Recover
Dealing with urinary leakage after prostate cancer treatment can feel isolating—but you’re not alone. With the right preparation, rehabilitation, and expert support, thousands of men regain bladder control and return to active lives.
👉 Ready to start your journey to recovery? Browse our Men’s Pelvic Health Programs .
This blog is part of our blog series on incontinence after prostate treatment. Be sure to check out our other blogs:
- Urinary incontinence after prostate surgery or radiation.
- Pelvic floor exercises after prostate surgery or radiation.
- Surgery to fix incontinence after prostate surgery or radiation.
Also, feel free to reach out to us at [email protected] for more education about pelvic floor health.